Following a successful heart valve replacement, it can be disappointing to hear news that one’s heart valve is failing again
Unfortunately, bioprosthetic or tissue (artificial valves constructed from animal based tissue) heart valves, while engineered like the human heart valve still suffer wear and tear and may require replacement after some time.
What causes this wear and tear to happen?
This could be an interplay of calcification (mineral formation) of the valve leaflets( causing stiffening), mechanical stress, lipid ( cholesterol) seeping into the valve tissue and immune response contributing to acceleration of valve damage. These conditions occur as there are marked biochemical and cell structural differences between the native ( the original valve we are born with) aortic valve when compared with a bioprosthetic ( artificial man made) heart valve.
The rate of degeneration is affected by several factors. One of these include the age of the patient. Younger patients tend to experience a higher rate of deterioration. Advanced kidney disease, a hormone condition called hyperparathroidism, pregnancy and hypertension can also be contributory factors. Additionally, smaller sized valves, the location of the valves (mitral worse than aortic valve) are also known factors. Patients with diabetes and high cholesterol levels may also be at risk.
Is there a way to stop this?
There is no known way to prevent degeneration however the following may help prevent other causes of damage or its complications
This includes
- Avoid chronic diseases like high cholesterol, diabetes and therefore the risks of renal failure by maintaining a healthy lifestyle
- Good dental hygiene. This is important as bacteria from mouth could get into the blood stream and infect the valve causing a serious condition called endocarditis. This is difficult to treat and requires prolonged antibiotics or even repeat operation if the valve becomes badly damaged.
- Antibiotic prophylaxis. Speak to your healthcare team to understand when you should be on antibiotics before any invasive procedure/dental work
- Follow up with your cardiologist. An echocardiogram may be needed to determine the status of the valve and the function of the heart.
- Be aware of changes in symptoms such as fatigue, breathlessness, chest pain, palpitations or leg swelling. These should not be dismissed without assessment.
‘My valve is badly damaged’ what options and alternatives do I have?
- The valve can be removed and replaced via repeat open surgery. You may wish to speak to your doctor about the options of biological versus mechanical valves and their durability.
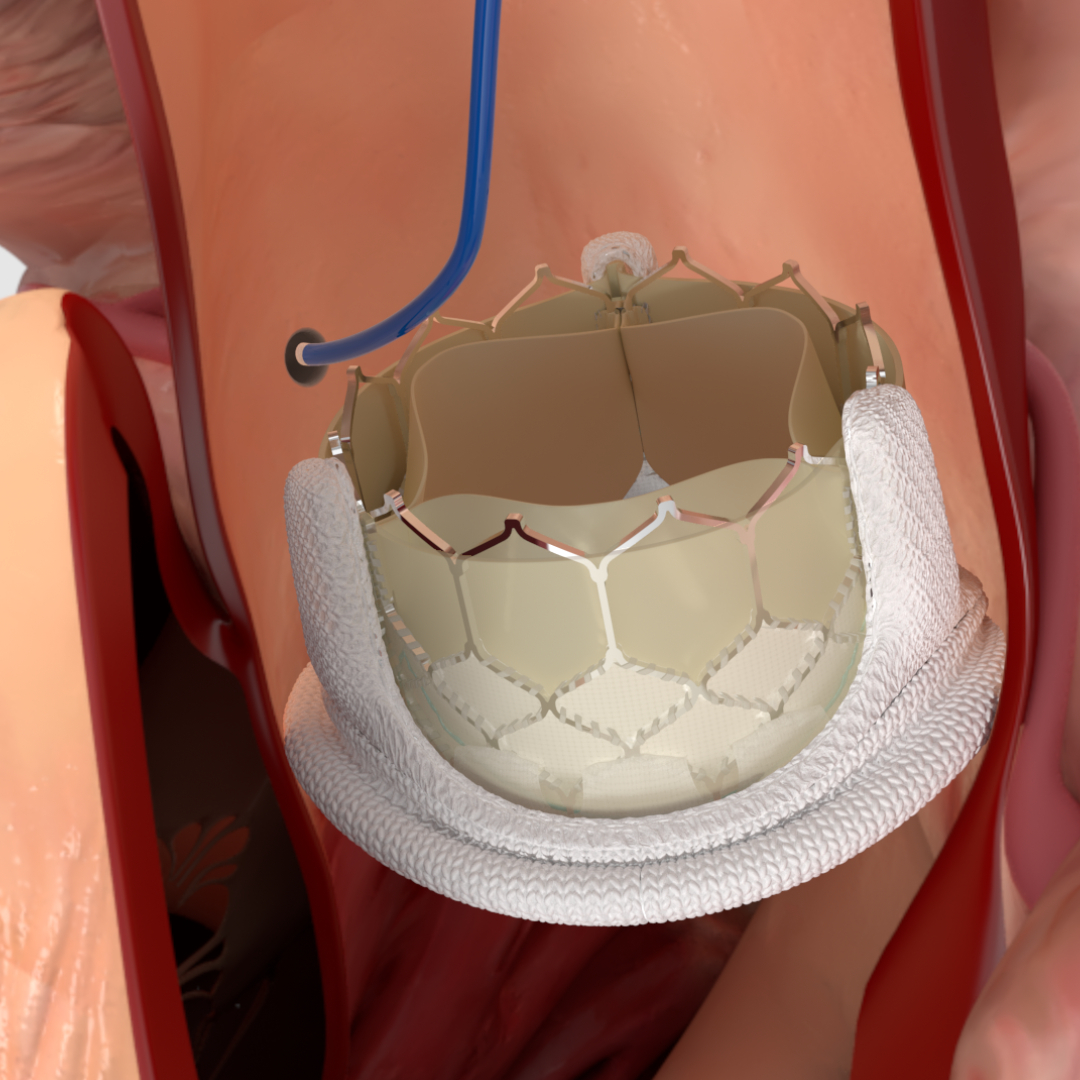
- There is now a new, much less invasive option of a valve-in-valve procedure for selected patients. This in particularly useful for those who are at high risk of a repeat operation. The new valve that is implanted is known as a transcatheter heart valve. The degenerated valve is not removed but instead, a stent-like valve is inserted through the thigh and this stent is deployed within the degenerated valve. This pushes the damaged valve tissues to the side while the new valve starts to function within immediately. This can be done with neither the need to stop the heart nor be placed on a heart lung machine. This is therefore more gentle and results in a significantly shortened recovery time and much less pain. It is important to understand that this transcatheter heart valve is also a biological valve, thus this too may degenerate over time but certainly adds and restores lifespan to the old valve
- Is there an option of medications alone? Medications may be used to reduce the symptoms that arise from the valve disease but will not influence the progression of the valve disease